Making Sense of Sgarbossa’s Criteria – Chest Pain and Left Bundle Branch Block – Part 2
 In Part 1 of this series we discussed why left bundle branch block presents a dilemma for clinicians who provide care for patients who suffer chest pain (or other signs and symptoms of ACS).
In Part 1 of this series we discussed why left bundle branch block presents a dilemma for clinicians who provide care for patients who suffer chest pain (or other signs and symptoms of ACS).
Now I’d like to talk about “new” left bundle branch block.
In practice this turns out to be “left bundle branch block not known to be old”. Let’s face it: how often do patients know they have a history of left bundle branch block? How often do we have an “old” ECG for comparison?
This was considered to be a STEMI equivalent as recently as the 2010 AHA ECC Guidelines!
Chest pain and new left bundle branch block, by itself, is no longer considered to be an indication for immediate reperfusion therapy.
How did we get here? Consider the following:
“Patients with new or presumably new left bundle-branch block had an inordinately high prevalence of false positive catheterization laboratory activation (almost half did not have a culprit artery).”
Larson, Menssen, Sharkey et al, False-Positive Cardiac Catheterization Laboratory Activation Among Patients With Suspected ST-Segment Elevation Myocardial Infarction, JAMA 2007;298(23):2754-2760.
“Despite guideline recommendations that patients with potential ACS and new or presumed new LBBB should be treated similar to STEMI, ED patients with a new or presumed new LBBB are not at increased risk of AMI. In fact, the presence of LBBB, whether new or old, did not predict AMI. Caution should be used in applying recommendations derived from patients with definite AMI to ED patients with potential ACS that may or may not be sustaining an AMI.”
Chang AM, Shofer FS, Tabas JA, et al. Lack of association between left bundle-branch block and acute myocardial infarction in symptomatic ED patients. Am J Emerg Med 2009;27:916-921
“New or presumably new LBBB has been considered a STEMI equivalent. Most cases of LBBB at time of presentation, however, are “not known to be old” because of prior electrocardiogram (ECG) is not available for comparison. New or presumably new LBBB at presentation occurs infrequently, may interfere with ST-elevation analysis, and should not be considered diagnostic of acute myocardial infarction (MI) in isolation.”
2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:00-00
If that’s all true then why was the presence of a “new” left bundle branch block considered a STEMI equivalent in the first place?
To answer that question we need to go back to the fibrinolytic trials of the 1980s.
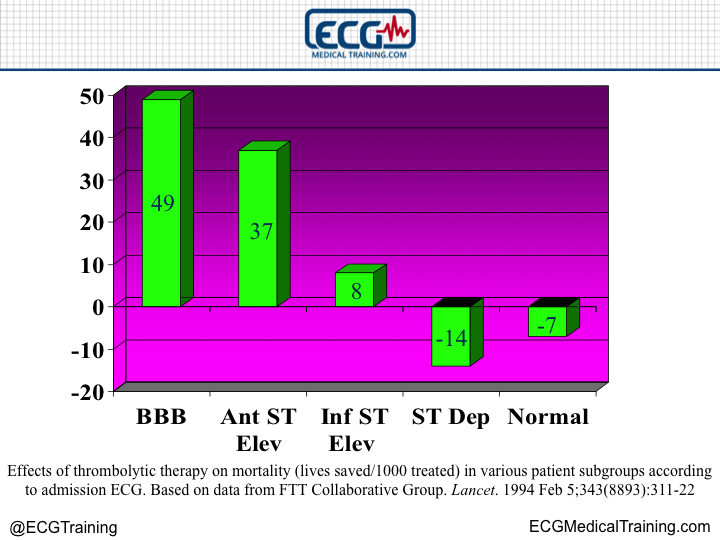
When FTT Collaborative Group analyzed thousands of patients from the fibrinolytic trials it turned out that, statistically speaking, patients with bundle branch blocks (you will notice I did not specifically say left bundle branch block) received the highest mortality benefit.
They did much better than say, patients with inferior ST-segment elevation. In hindsight this is surprising!
Keep in mind that these trials did not confirm acute myocardial infarction with angiography, but rather, a rise and fall of cardiac biomarkers. As a consequence they combined STEMI and NSTEMI.
In 1996 the GUSTO-I investigators including Elena Sgarbossa, M.D. published a very well known study in the New England Journal of Medicine that attempted to elucidate the ECG features of acute, evolving MI in the presence of left bundle branch block.
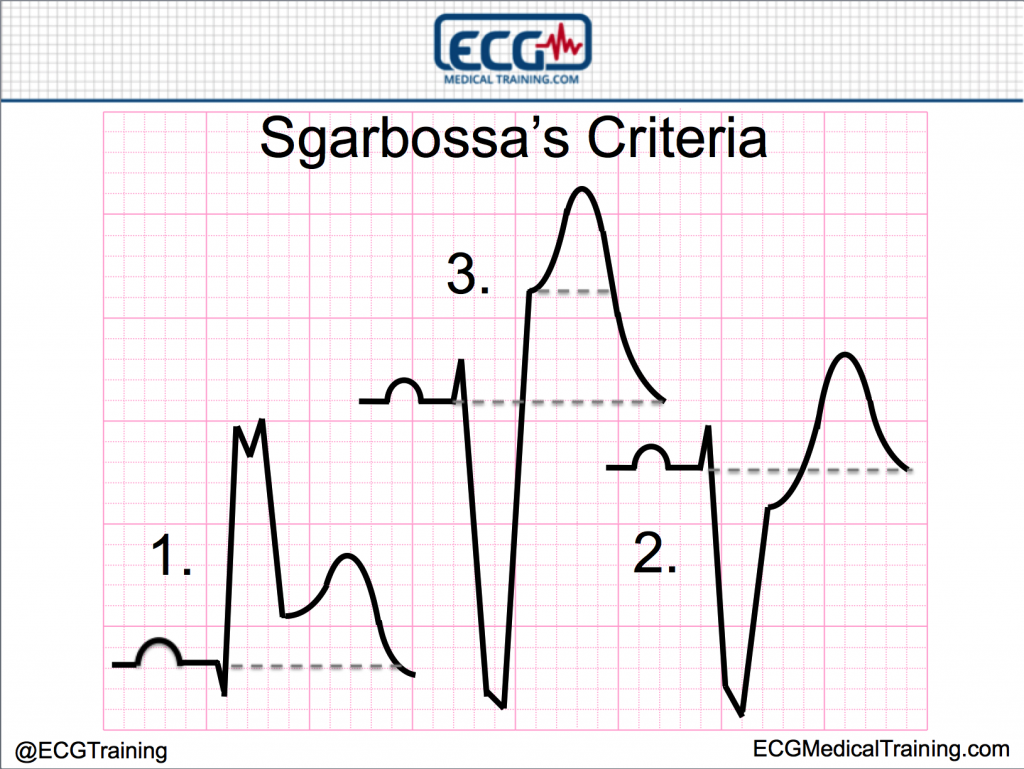
These features included:
- Concordant ST-elevation (ST-elevation in the same direction as the majority of the QRS complex)
- Concordant ST-depression (ST-depression in the same direction as the majority of the QRS complex in leads V1, V2, or V3)
- Discordant ST-segment elevation ≥ 5 mm
It was actually a scoring system. The more criteria that were met, the higher the probability that the patient was suffering acute myocardial infarction.
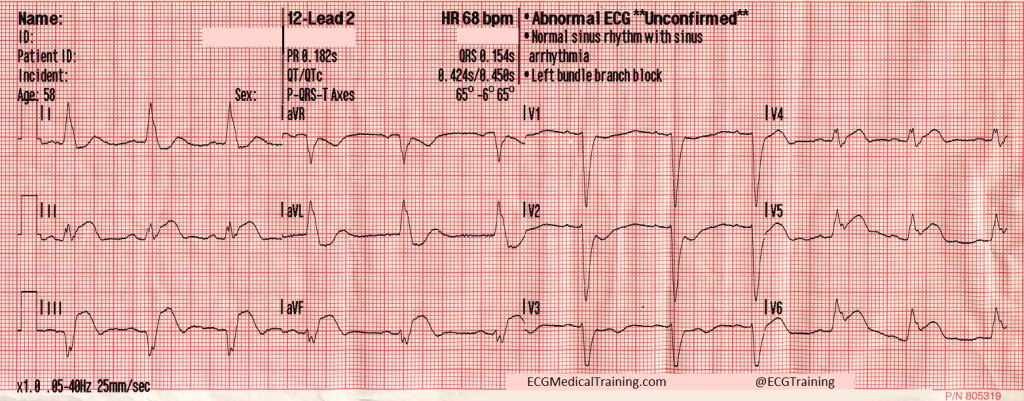
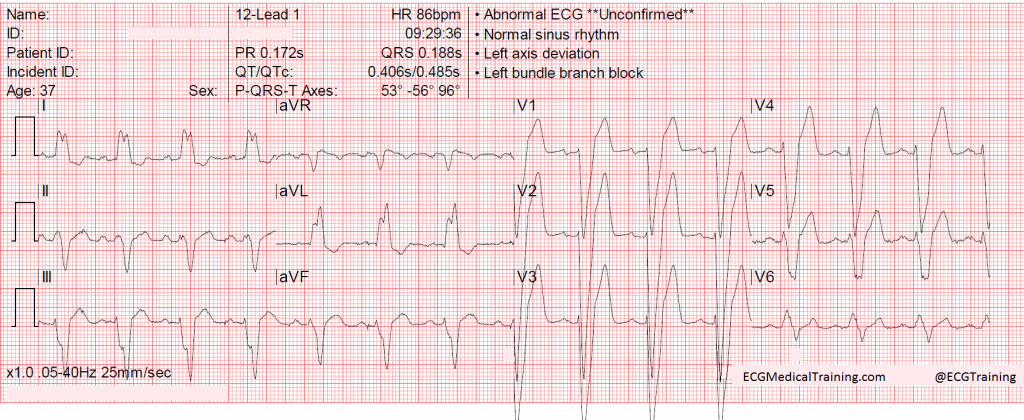
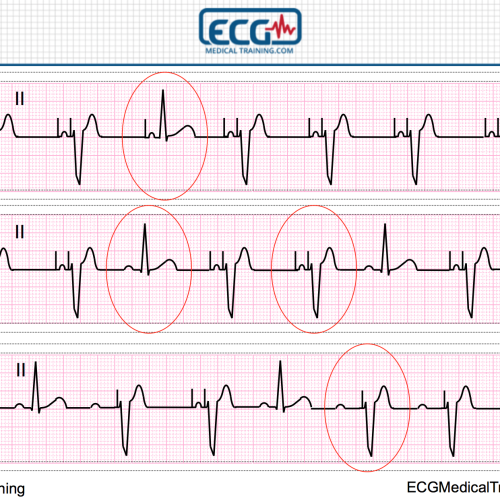
These criteria have been useful in detecting acute inferior, posterior, and lateral STEMI in the presence of left bundle branch block. Let’s look at an example.
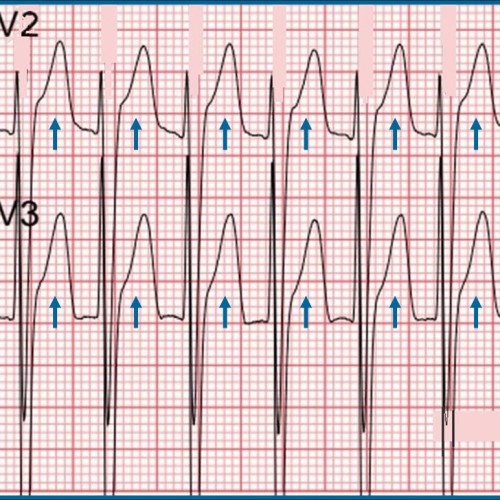
In this example we have concordant ST-elevation in leads II, V5, and V6 and concordant ST-depression in lead V1, V2, and V3. Sgarbossa’s original criteria do a pretty good job of detecting this type of STEMI.
It is the third criterion (discordant ST- elevation ≥ 5 mm) which has caused the most controversy. There are two reasons for this. First, the criterion is not particularly sensitive. Second, it is not particularly specific because GUSTO-I investigators did not take into account the rule of proportionality. In other words, the “5 mm rule” was absolute and did not take into account the depth of the S-wave.
Let me show you why this is a problem.
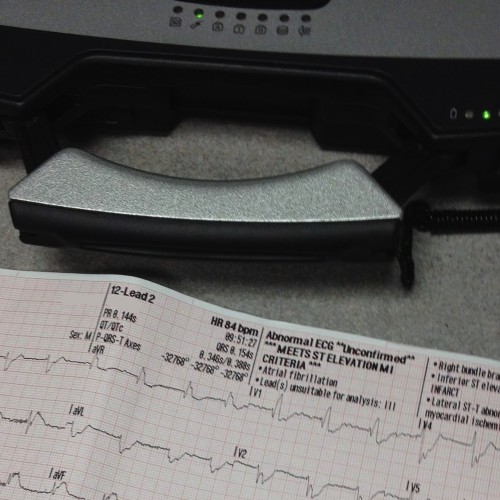
This patient presented to the emergency department with chest pain, left bundle branch block, and > 5 mm of ST-elevation in leads V2 and V3. But it wasn’t a STEMI.
The S-waves in lead V2 are 37 mm deep (the S-waves in lead V3 go off the bottom of the paper). This is an appropriate amount of discordant ST-elevation relative to the depth of the S-wave (the rule of proportionality). I have several other examples in my collection.
In fairness to Dr. Sgarbossa this would have only scored a 2 in her system for a 50% probability that the patient was suffering acute myocardial infarction. However, the consequence of this problem is that clinicians lost faith in this criterion and stopped applying it altogether.
I frequently hear from my colleagues in both Emergency Medicine and Cardiology that “all you need is concordance” when it comes to left bundle branch block. But if that’s true we’re writing off LAD occlusion because we see negative QRS complexes in leads V1-V4 in the setting of left bundle branch block.
If we’re not considering discordant ST-elevation in those leads we’re going to miss anterior STEMI. How do we solve this difficulty?
In Part 3 we’ll look at Smith’s modification to Sgarbossa’s criteria and discuss the importance of changes on serial ECGs!
Making Sense of Sgarbossa’s Criteria – Chest Pain and Left Bundle Branch Block – Part 1
Making Sense of Sgarbossa’s Criteria – Chest Pain and Left Bundle Branch Block – Part 2
Making Sense of Sgarbossa’s Criteria – Chest Pain and Left Bundle Branch Block – Part 3
References
Cai Q, Mehta N, Sgarbossa E et al. The left bundle-branch block puzzle in the 2013 ST-elevation myocardial infarction guideline: From falsely declaring emergency to denying reperfusion in a high-risk population. Are the Sgarbossa Criteria ready for prime time?. American Heart Journal. 2013;166(3):409-413. doi:10.1016/j.ahj.2013.03.032.
Chang A, Shofer F, Tabas J, Magid D, McCusker C, Hollander J. Lack of association between left bundle-branch block and acute myocardial infarction in symptomatic ED patients. The American Journal of Emergency Medicine. 2009;27(8):916-921. doi:10.1016/j.ajem.2008.07.007.
Garcia T, Holtz N. 12 Lead ECG: The Art of Interpretation. Boston, Ma: Jones and Bartlett; 2001.
Larson D, Menssen K, Sharkey S et al. “False-Positive” Cardiac Catheterization Laboratory Activation Among Patients With Suspected ST-Segment Elevation Myocardial Infarction. JAMA. 2007;298(23):2754. doi:10.1001/jama.298.23.2754.
Meyers H, Limkakeng A, Jaffa E et al. Validation of the modified Sgarbossa criteria for acute coronary occlusion in the setting of left bundle branch block: A retrospective case-control study. American Heart Journal. 2015;170(6):1255-1264. doi:10.1016/j.ahj.2015.09.005.
O’Gara P, Kushner F, Ascheim D et al. 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2012;127(4):e362-e425. doi:10.1161/cir.0b013e3182742cf6.
Smith S, Dodd K, Henry T, Dvorak D, Pearce L. Diagnosis of ST-Elevation Myocardial Infarction in the Presence of Left Bundle Branch Block With the ST-Elevation to S-Wave Ratio in a Modified Sgarbossa Rule. Annals of Emergency Medicine. 2012;60(6):766-776. doi:10.1016/j.annemergmed.2012.07.119.
Surawicz B, Knilans T, Chou T. Chou’s Electrocardiography In Clinical Practice. Philadelphia: Saunders; 2001.
Sgarbossa E, Pinski S, Barbagelata A et al. Electrocardiographic Diagnosis of Evolving Acute Myocardial Infarction in the Presence of Left Bundle-Branch Block. New England Journal of Medicine. 1996;334(8):481-487. doi:10.1056/nejm199602223340801.
Content Reviewer
Stephen Smith, M.D. (@SmithECGBlog)