SVT, Adenosine, and Postural Modification to the Valsalva Maneuver (REVERT Trial)
EMS is called to the clubhouse of a golf course for a female patient in her early 50s complaining of palpitations.
She had just finished playing 18 holes when her “heart started racing”. She has a history of supraventricular arrhythmias and reportedly attempted vagal maneuvers prior to EMS arrival without success.
Aside from occasional arrhythmias the patient is healthy and takes no prescription medications. She states that her personal physician has considered placing her on a beta blocker in the past. She is allergic to penicillin.
The patient’s skin is pink, moist, and very warm. She denies chest pain but admits to feeling breathless.
Breath sounds are clear and equal bilaterally.
Vital signs are assessed.
- RR: 18
- HR: 200
- NIBP: 138/100
- Temp: 98.9 F / 37.2 C
- SpO2: 97% on room air
The cardiac monitor is attached.
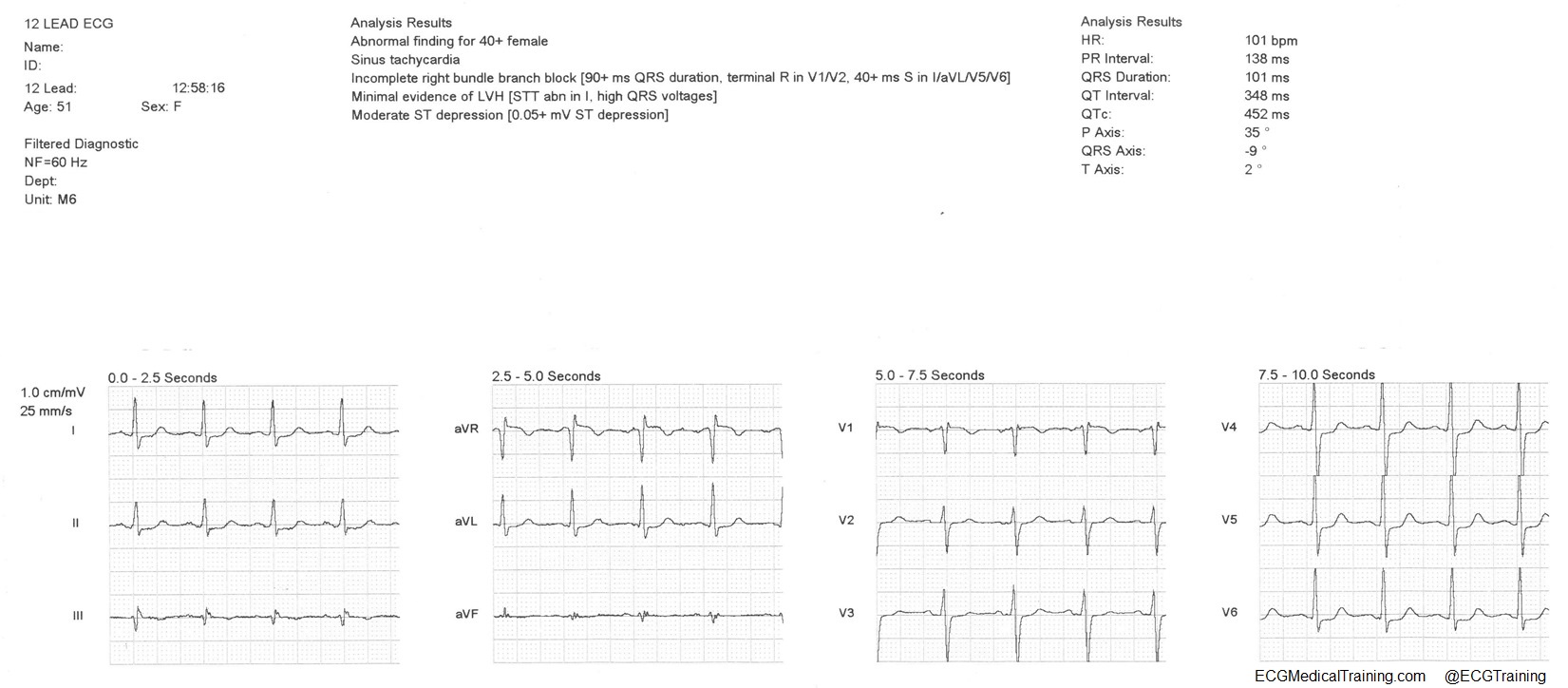
A 12-lead ECG is obtained.
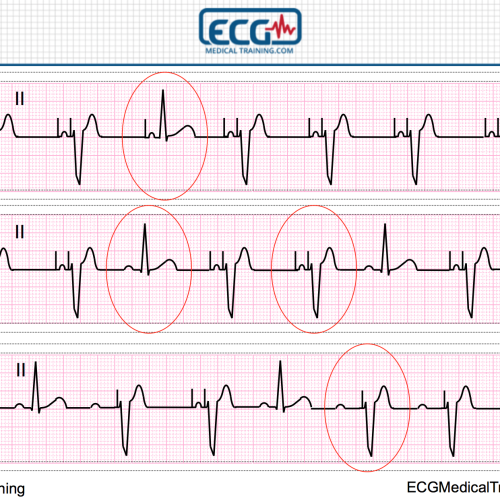
There is a regular narrow complex tachycardia at a rate of 191. There are no visible P-waves. This is likely AV nodal reentrant tachycardia (AVNRT) or orthodromic AV reentrant tachycardia (AVRT).
Paramedics attempt a postural modification to the Valsalva maneuver as described in the REVERT Trial.
During the “strain phase” (A.) the patient is placed in high Fowlers, given a 10 ml syringe, and encouraged to blow continuously into the syringe, displacing the plunger, for approximately 15 seconds. During the “relaxation phase” (B.) the patient is laid supine and the legs are manually elevated.
You can see a video of the technique here.
In the REVERT Trial the standard technique returned 17% of patients to sinus rhythm, whereas the modified technique returned 43% of patients to sinus rhythm — more than doubling the effectiveness!
Unfortunately, in this case the maneuver was attempted twice without success.
Additional Treatments
- Defibrillation pads were applied.
- IV access was achieved.
- 6 mg of adenosine was given rapid IV push followed by a 20 ml bolus of normal saline.
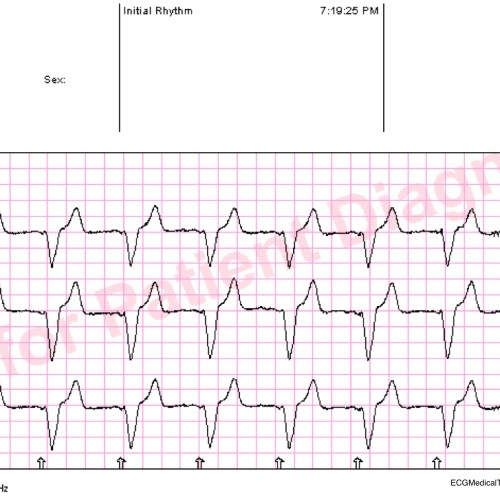
The heart rhythm converts to sinus tachycardia.
However, the patient continued to feel “breathless”.
A post-conversion 12-lead ECG is obtained.
There is modest ST-segment elevation in lead aVR with widespread ST-segment depression. It could easily be residual demand-side ischemia from the rapid heart rate.
The patient briefly considered refusing transport to the Emergency Department.
I am aware of one trial from the UK where it was shown that paramedic treatment and discharge of patients with regular SVT is safe, efficacious and reduces admissions (when the patient is hemodynamically stable and has no history of structural or ischemic heart disease).
However, this was a beyond the comfort level of the treating paramedics, especially since the patient continued to feel breathless. After a brief discussion the patient agreed to be transported to the hospital for further testing and observation.
References
Appelboam A, Reuben A, Mann C et al. Postural modification to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias (REVERT): a randomised controlled trial. The Lancet. 2015;386(10005):1747-1753.
Baker A, Whitbread M, Richmond L et al. Safety and efficacy of paramedic treatment of regular supraventricular tachycardia. Heart. 2013;99(suppl 2):A46.1-A46.
Further Reading