Making Sense of Sgarbossa’s Criteria – Chest Pain and Left Bundle Branch Block – Part 3
 In this final part of the series I’d like to talk about Smith’s modification to Sgarbossa’s criteria (PDF) and the importance of serial ECGs.
In this final part of the series I’d like to talk about Smith’s modification to Sgarbossa’s criteria (PDF) and the importance of serial ECGs.
If you recall there are two main problems with using 5 mm as an arbitrary cut-off for discordant ST-elevation in the presence of left bundle branch block.
First, not all coronary occlusions will present with 5 mm of discordant ST-elevation (a problem with sensitivity). Second, many patients with 5 mm of discordant ST-elevation are not suffering acute STEMI (a problem with specificity).
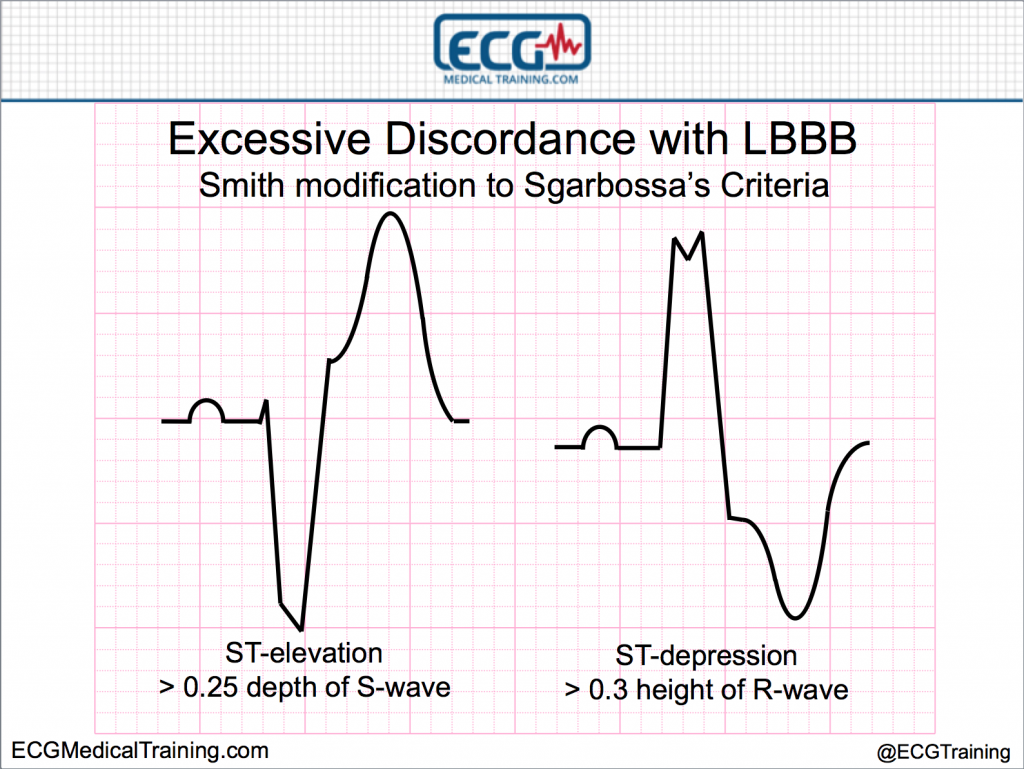
Smith’s modification to Sgarbossa’s criteria
Stephen Smith, M.D. and his colleagues helped solve this difficulty by using the rule of proportionality and introducing the concept of excessive discordance relative to the depth of the S-wave (the ST/S ratio).
ST-elevation is “excessively discordant” when the ST-elevation (measured at the J-point) is > 0.25 or 25% the depth of the S-wave.
ST-depression is “excessively discordant” when the ST-depression (measured at the J-point) is > 0.3 or 30% the height of the R-wave.
Let’s look at an example.
This was an 80 year old male with a chief complaint of chest pain.
The 12-lead ECG shows left bundle branch block.
Discordant ST-elevation > 5 mm is present in leads V1, V2, V3, and V4. But is it excessively discordant? After all, the S-wave in lead V2 is at least 35 mm deep!
If you break out the calipers here are the measurements.
Lead V1
S-wave: 18 mm
ST-elevation at J-point: 6 mm
ST/QRS ratio: -0.33 (positive)
Lead V2
S-wave: 37 mm
ST-elevation at J-point: 10 mm
ST/QRS ratio: -0.27 (positive)
Leave V3
S-wave cut off by bottom of ECG paper
Lead V4
S-wave: 23 mm
ST-elevation at J-point: 7 mm
ST/QRS ratio: -0.3 (positive)
Lead V6
R-wave: 10 mm
ST-depression at J-point: 3 mm
ST/QRS ratio: -0.3 (positive)
So Smith’s modified rule correctly predicts LAD occlusion for this case; but if you’re like me, you’re not about to break out a set of calipers in the back of the ambulance!
As a practical matter I allow 1 mm of ST-elevation for every large block (5 mm) of S-wave depth (and I round up). Let me show you how this works.
In lead V2 there are 7 large blocks of S-wave depth plus a couple of mm so I round up to 8 large blocks. Now I will “allow” up to 8 mm of ST-elevation in this lead. As you can see there are 10 mm of ST-elevation so this is suspicious for acute injury.
Keep in mind that I am still going to have to “sell” this to an ED physician because our Code STEMI protocol excludes patients with left bundle branch block! The important thing, in my view, is to deliver these patients directly to PCI hospitals.
It’s one thing to identify a patient suffering LAD occlusion in the presence of left bundle branch block. It’s another to persuade a decision maker to activate the cardiac cath lab!
See also
New Left Bundle Branch Block (LBBB) and Dyspnea at Dr. Smith’s ECG Blog
Chest pain, left bundle branch block, and excessively discordant ST-segment elevation at EMS 12-Lead
A word of caution for heart failure patients in pulmonary edema
When using Smith’s modification I have been fooled twice when I applied it to patients with heart failure, paced rhythm, hypertension, and acute pulmonary edema.
Once the patients received nitroglycerin and CPAP the ST-segments came down and they were no longer excessively discordant. I know we haven’t even discussed using Sgarbossa’s criteria in the setting of paced rhythm as distinguished from left bundle branch block but it’s just something to be aware of.
Update: I received this helpful comment from Stephen Smith, M.D.: “We specifically excluded patients with pulmonary edema because 1.) I noticed that they have false positives. 2.) They are likely to need intensive therapy and evaluation anyway.”
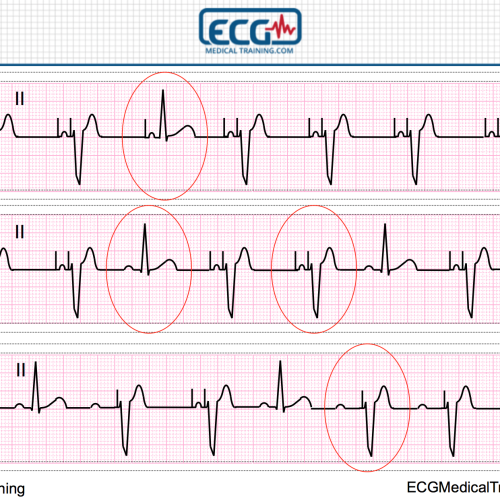
The importance of serial ECGs
As a final thought, when it comes to STEMI recognition the importance of recognizing changes on serially obtained ECGs cannot be overemphasized.
Let’s look at another example.
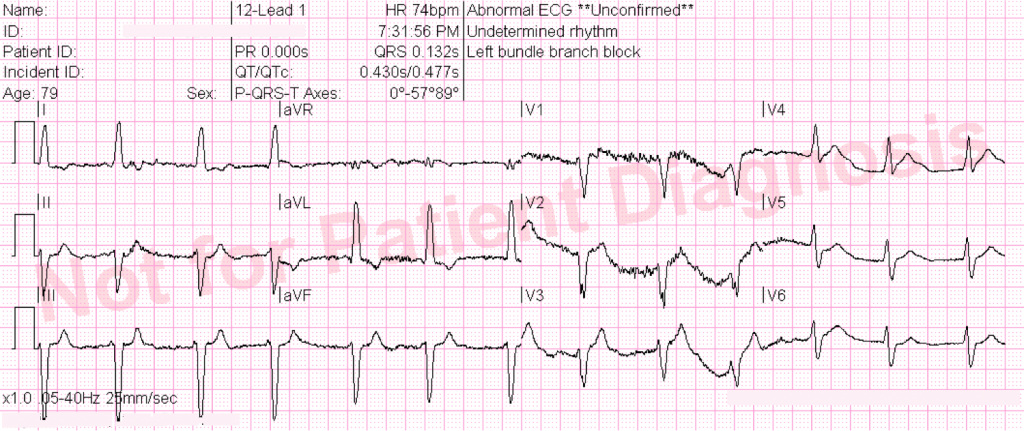
This was a 79 year old who complained of chest pain.
This is the first prehospital 12-lead ECG of two. The data quality isn’t that great (and we could debate as to whether or not it’s a supraventricular rhythm) but the QRS is “wide” at 132 ms and shows LBBB morphology.
It is nondiagnostic for acute STEMI.
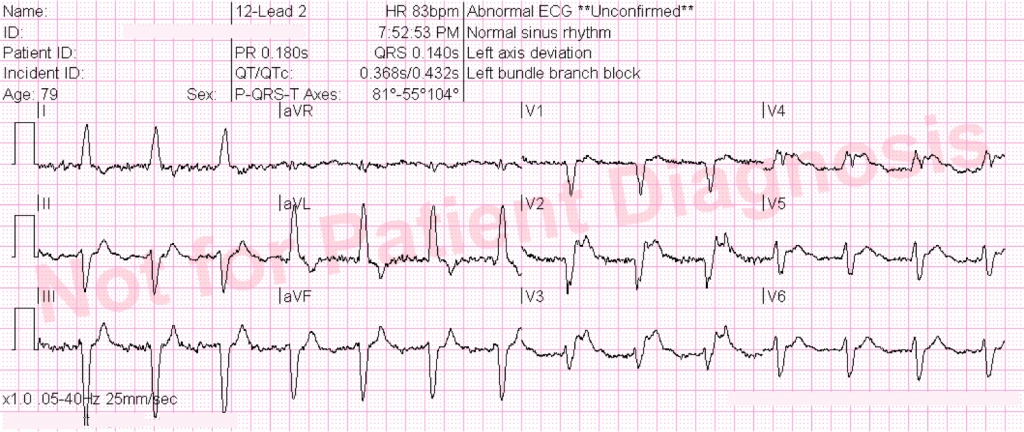
A second 12-lead ECG was printed out in the back of the ambulance on arrival at the hospital. Now does it show acute STEMI? The answer is yes!
There is now excessively discordant ST-elevation in leads V2 and V3 and concordant ST-elevation in lead V4. Unfortunately, the patient suffered cardiac arrest prior to cardiac cath and was not successfully resuscitated.
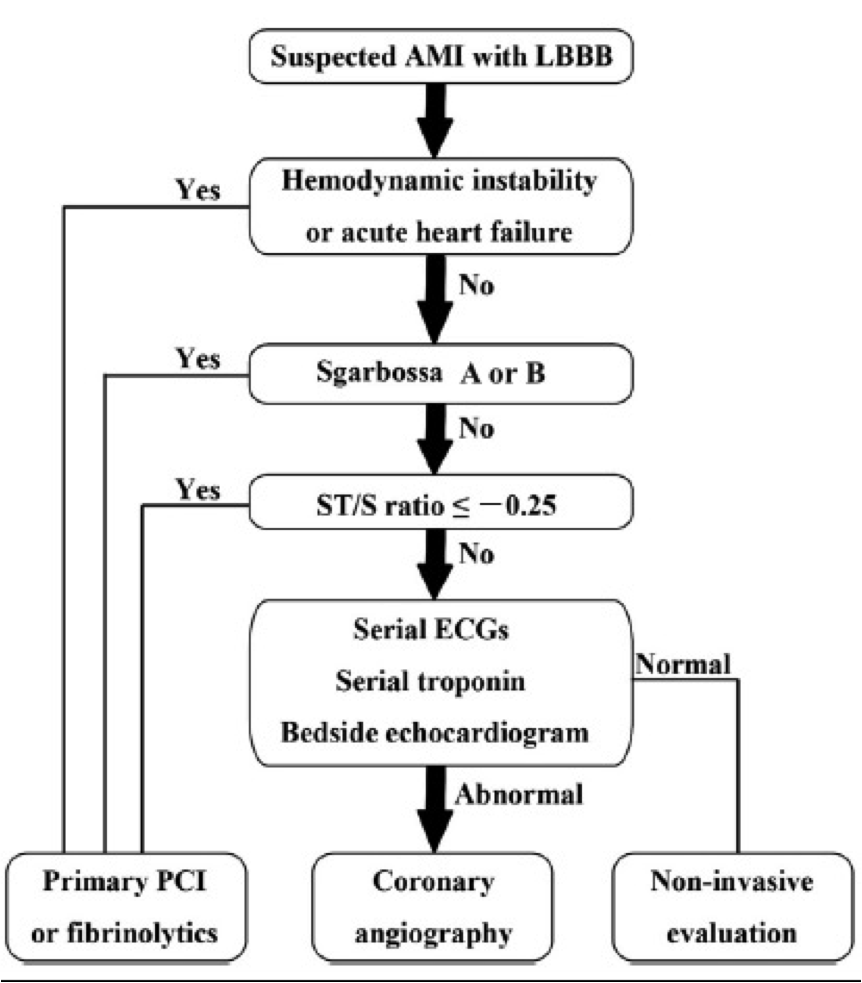
Which patients with chest pain and left bundle branch block should receive primary PCI?
This question was recently answered in an article in the American Heart Journal that merged together clinical instability or acute heart failure, Sgarbossa A or B (concordant ST-elevation or concordant ST-depression), ST/QRS ratio > -0.25 (Smith’s modification of Sgarbossa’s criteria), serial ECGs, serial cardiac biomarkers, and bedside echocardiogram.
Conclusion
Evaluating patients with chest pain and left bundle branch block can be challenging but a correct understanding of the 12-lead ECG can be valuable in triage, treatment, and transfer decisions.
Making Sense of Sgarbossa’s Criteria – Chest Pain and Left Bundle Branch Block – Part 1
Making Sense of Sgarbossa’s Criteria – Chest Pain and Left Bundle Branch Block – Part 2
Making Sense of Sgarbossa’s Criteria – Chest Pain and Left Bundle Branch Block – Part 3
References
Cai Q, Mehta N, Sgarbossa E et al. The left bundle-branch block puzzle in the 2013 ST-elevation myocardial infarction guideline: From falsely declaring emergency to denying reperfusion in a high-risk population. Are the Sgarbossa Criteria ready for prime time?. American Heart Journal. 2013;166(3):409-413. doi:10.1016/j.ahj.2013.03.032.
Chang A, Shofer F, Tabas J, Magid D, McCusker C, Hollander J. Lack of association between left bundle-branch block and acute myocardial infarction in symptomatic ED patients. The American Journal of Emergency Medicine. 2009;27(8):916-921. doi:10.1016/j.ajem.2008.07.007.
Garcia T, Holtz N. 12 Lead ECG: The Art of Interpretation. Boston, Ma: Jones and Bartlett; 2001.
Larson D, Menssen K, Sharkey S et al. “False-Positive” Cardiac Catheterization Laboratory Activation Among Patients With Suspected ST-Segment Elevation Myocardial Infarction. JAMA. 2007;298(23):2754. doi:10.1001/jama.298.23.2754.
Meyers H, Limkakeng A, Jaffa E et al. Validation of the modified Sgarbossa criteria for acute coronary occlusion in the setting of left bundle branch block: A retrospective case-control study. American Heart Journal. 2015;170(6):1255-1264. doi:10.1016/j.ahj.2015.09.005.
O’Gara P, Kushner F, Ascheim D et al. 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2012;127(4):e362-e425. doi:10.1161/cir.0b013e3182742cf6.
Smith S, Dodd K, Henry T, Dvorak D, Pearce L. Diagnosis of ST-Elevation Myocardial Infarction in the Presence of Left Bundle Branch Block With the ST-Elevation to S-Wave Ratio in a Modified Sgarbossa Rule. Annals of Emergency Medicine. 2012;60(6):766-776. doi:10.1016/j.annemergmed.2012.07.119.
Surawicz B, Knilans T, Chou T. Chou’s Electrocardiography In Clinical Practice. Philadelphia: Saunders; 2001.
Sgarbossa E, Pinski S, Barbagelata A et al. Electrocardiographic Diagnosis of Evolving Acute Myocardial Infarction in the Presence of Left Bundle-Branch Block. New England Journal of Medicine. 1996;334(8):481-487. doi:10.1056/nejm199602223340801.
Content Reviewer
Stephen Smith, M.D. (@SmithECGBlog)